Autor : Abrate, Vanesa1, CarlĂ©s, Daniel2, Khoury, Marina3, LĂłpez, Ana MarĂa1, Ortiz, MarĂa Cristina5, Wustten, Sebastián6
1 Hospital Universitario Privado de CĂłrdoba,
2Pulmonologist, Chaco,
3Medical Research Institute Alfredo Lanari, University of Buenos Aires,
5Pulmonologist, province of Buenos Aires,
6Hospital San MartĂn, Paraná; Hospital Cullen, Santa Fe
Clinical and Critical Care Section of the AAMR
https://doi.org/10.56538/ramr.ESNJ3391
Correspondencia : Vanesa Abrate. E-mail: abrate.vanesa@gmail.com
ABSTRACT
Introduction: Since there are various guidelines for respiratory diseases, we aimed to
know which are chosen by physicians in their daily clinical practice.
Methods: A descriptive, cross-sectional study was conducted through a
questionnaire sent to pulmonologists of the Argentinian Association of
Respiratory Medicine.
Results: The most commonly used guideline for COPD (chronic obstructive pulmonary
disease) was the Global Initiative for Chronic Obstructive Lung Disease (GOLD)
(82 %), followed by GesEPOC (51 %). For asthma, the most commonly used guideline was the Global Initiative
for Asthma (GINA) 2022 (89 %) and the Spanish Guideline on the Management of
Asthma (known for its acronym in Spanish, GEMA), GEMA 5.2 (68 %). In
difficult-to-control asthma, GINA 2022 (82 %) and GEMA 2022 (53 %) were used.
With regard to spirometries, 54 % of respondents
favored NHANES III (Third National Health and Nutrition Examination Survey) and
22 % used theoretical Knudson reference values. For pneumonia, 62 % chose the
guidelines of the SADI (Argentinian Society of Infectious Diseases), 37 %
preferred those of the IDSA (Infectious Diseases Society of America) and 20 %,
chose the guidelines of the BTS (British Thoracic Society). For pulmonary
nodules, 62 % used Fleischner guidelines, and 35 %
favored Lung-RADS 1.1. For hypersensitivity pneumonitis, 83 % selected the
ATS/JRS/ALAT Guidelines (American Thoracic Society/Japanese Respiratory
Society/Latin American Thoracic Society). And with respect to pulmonary
fibrosis imaging, 89 % used ALAT/ERS (EuÂropean Respiratory Society)/JRS
recommendations, and 18 % preferred White Paper.
Discussion: Although there are studies about adherence to guidelines, none of them
shows which are the chosen recommendations within a group of
guidelines of the same topic. In COPD and asthma (including
difficult-to-control asthma) GOLD, GINA and the guidelines of the Spanish
Society of Respiratory Disease (GesEPOC and GEMA)
were chosen. The preference for the national guideline for pneumonia is
consistent with the need to consider local epidemiology.
Key words: Clinical Practice Guidelines, Respiratory Tract Diseases, GOLD, GesEPOC, GINA, GEMA
RESUMEN
IntroducciĂłn:
Dada
la existencia de variadas guĂas para enfermedades respiratorias, se buscĂł conocer
cuáles eligen los mĂ©dicos para utilizar en su práctica clĂnica.
Materiales
y MĂ©todos: se
realizĂł un estudio descriptivo, transversal, mediante una encuesta a neumonĂłlogos de la AsociaciĂłn Argentina de Medicina
Respiratoria.
Resultados:
La
guĂa más utilizada para EPOC fue la Iniciativa Global para la EnfermeÂdad
Pulmonar Obstructiva CrĂłnica (GOLD) (82 %), seguida por GesEPOC
(51 %). Para asma las más usadas fueron la Iniciativa Global para el Asma
(GINA) 2022 (89 %) y GEMA 5.2 (68 %). En asma de difĂcil control, se
prefirieron GINA 2022 (82 %) y GEMA 2022 (53 %). En espirometrĂa,
un 54 % de los respondedores se inclinĂł por NHANES III y un 22 % utilizĂł
valores teĂłricos de referencia de Knudson. En
neumonĂa, el 62 % eligiĂł SADI, el 37 %, IDSA y el 20 %, BTS. Para nĂłdulos
pulmonares, el 62 % prefiriĂł las guĂas Fleischner, 35
% se inclinĂł por Lung-RADS 1.1. Para neumonitis por
hipÂersensibilidad, un 83 % seleccionĂł las guĂas de las sociedades conjuntas
ATS/JRS/ ALAT. Para imágenes de fibrosis pulmonar, el 89 % utilizó
ALAT/ERS/JRS/ALAT y el 18 % White Paper.
DiscusiĂłn:
Si
bien hay estudios sobre adherencia a guĂas, no los hay acerca de preferencias
de utilizaciĂłn entre varias referidas a un mismo tema. En EPOC y asma
(incluyendo la de difĂcil control) se eligieron GOLD y GINA y las de la
Sociedad Española de PatologĂa Respiratoria (GesEPOC
y GEMA). El uso preferencial de la guĂa nacional para neumonĂa es coherente con
la necesidad de contemplar la epidemiologĂa local.
Palabras
clave: GuĂas
de práctica clĂnica, Enfermedades respiratorias, GOLD, GesEPOC,
GINA, GEMA
Received: 09/25/2023
Accepted: 02/05/2024
INTRODUCTION
Clinical practice guidelines
provide a set of standards of care for the diagnosis and treatment of various diseases.
The most common respiratory diseases are addressed by different guidelines,
both national and international. These guidelines are periodically updated
based on new evidence and are advisory in nature for practice.1
Their recipients vary from general
physicians to specialists. Although they may be thought of as opposed to
personalized medicine trends, they actually complement each other since the
application of a guideline is never automatic; it requires taking into account
the characteristics of the patient and their context.1,2 The guidelines themÂselves are the result of
systematic reviews; expert consensus is involved, both in the stage of choosing
the most appropriate questions and in evaluating the results obtained and the
final recommendations.3 Many medical
specialty congresses dedicate part of their time to presenting, discussing, or
updatÂing them, contributing to their dissemination and eventual use.
From the Clinical and Critical
Care Section of the Argentinian Association of Respiratory MediÂcine (AAMR), we
aim to understand which are the specialty guidelines
chosen by pulmonologists asÂsociated with the AAMR.
MATERIALS AND METHODS
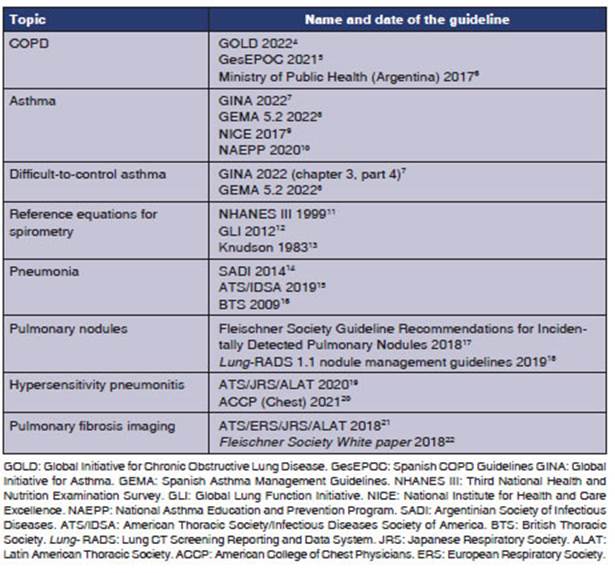
A cross-sectional study was
conducted through an anonÂymous survey of the physicians who are members of the
AAMR. A questionnaire was designed using a form on the Survey Monkey©
platform which included questions about the characteristics of the physicians
and their use of pulmonology guidelines. The researchers selected the most widely
disseminated guidelines for relevant respiratory diseases and other respiratory
topics (Table 1) based upon their criteria. The survey allowed respondents to
select more than one guideline for each topic, because in practiÂce, physicians
make use of elements from one guideline or another, according to their needs.
With the agreement of the AAMR
authorities, 946 active members of the updated roster of pulmonologists as of OctoÂber
25, 2022 were invited to participate via email. Between October 25 and December
15, 2022, the questionnaires were sent out initially and resent up to a maximum
of four times to those who did not respond.
The analysis was conducted using Stata 16.0 software (StataCorp,
Texas, USA). Groups were compared using the chi-square test or Fisher’s exact
test, as appropriate. A p-value of <0.05 was considered significant.
RESULTS
318 completed forms were
obtained, resulting in a response rate of 33.61 %. The characteristics of the
sample are presented in Table 2.
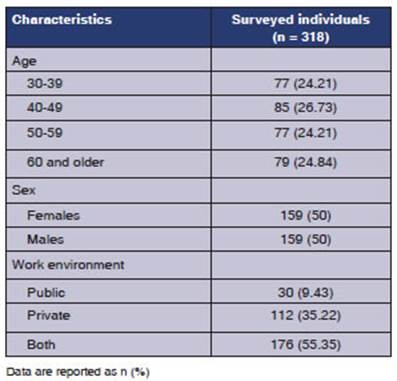
A higher proportion of women was found among respondents under 50 years of age. 59.26 %
(n = 96) of the 162 respondents under 50 years of age and 40.38 % (n = 62) of
the 156 respondents aged 50 or older were women. This difference was
statistically significant (p = 0.001).
Although the public sector as the
sole workÂplace was underrepresented, women and responÂdents under 50 years of
age were predominant in that sector. 73.33 % (n = 22) of the 30 responÂdents
who worked solely in the public sector, 43.75 % (n = 49) of the 112 who worked
in the private sector, and 50 % (n = 88) of the 176 who worked in both sectors
were women (p = 0.016). Similarly, 66.67 % (n = 20) of the 30 respondents who
worked solely in the public sector, 39.29 % (n = 44) of the 112 of the private
sector, and 55.68 % (n = 98) of the 176 respondents who worked in both sectors were under 50 years of age (p = 0.005).
It was common for the
respondents to select more than one guideline for each condition. Table 3 shows
the reported frequency of use for each guideline.
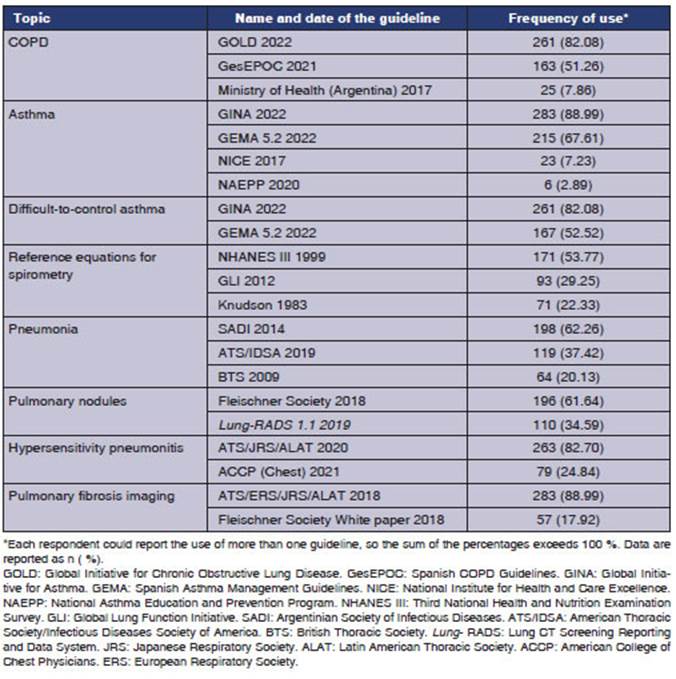
In COPD, the most
commonly used guideline was the GOLD (82 %), followed by GesEPOC
(51 %); and the least consulted was the one from the Ministry of Health of the
Nation (8 %). For asthma, the most frequently chosen guidelines were GINA 2022
(89 %), GEMA 5.2 (68 %), NICE (7 %), and NAEPP (2 %). In difficult-to-control
asthma, GINA 2022 (82 %) and GEMA 2022 (53 %) were mostly used. In relation to spirometries, 54 % of respondents chose NHANES III and 22 %
used theoretical Knudson reference values. For pneuÂmonia, 62 % chose the
guidelines of the SADI, 37 % preferred those of the IDSA and 20 %, chose the
BTS. For pulmonary nodules, 62 % of respondents used Fleischner
guidelines, and 35 % favored Lung-RADS 1.1. For hypersensitivity pneumonitis,
83 % selected the ATS/JRS/ALAT Guidelines, and 25 % chose the AACP (American
Association of Chest Physicians). Regarding pulmonary fibrosis imaging, 89 %
used ALAT/ERS/JRS recommendaÂtions, and 18 % preferred White Paper.
Table 4 compares the
use of guidelines across groups according to gender.
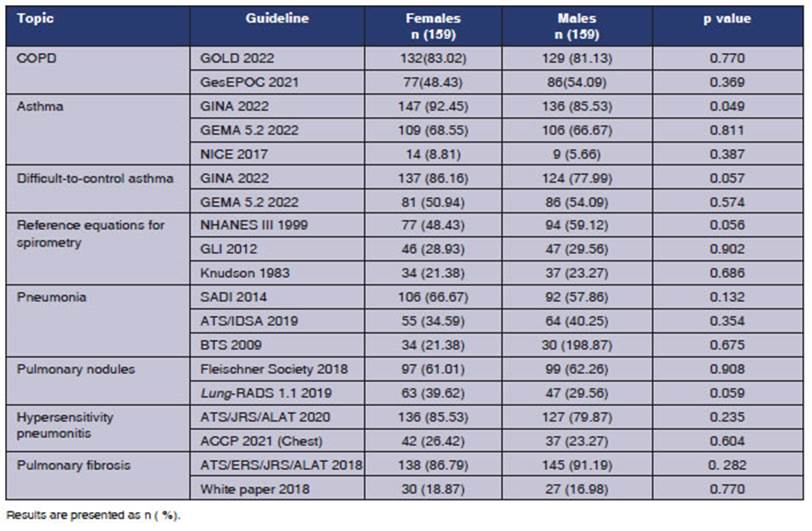
There were no
differences across the groups according to gender in the frequency of use of
most guidelines, with the exception that women reported a higher frequency in the
use of the GINA guidelines for asthma.
Table 5 compares the use of
guidelines across groups according to age.
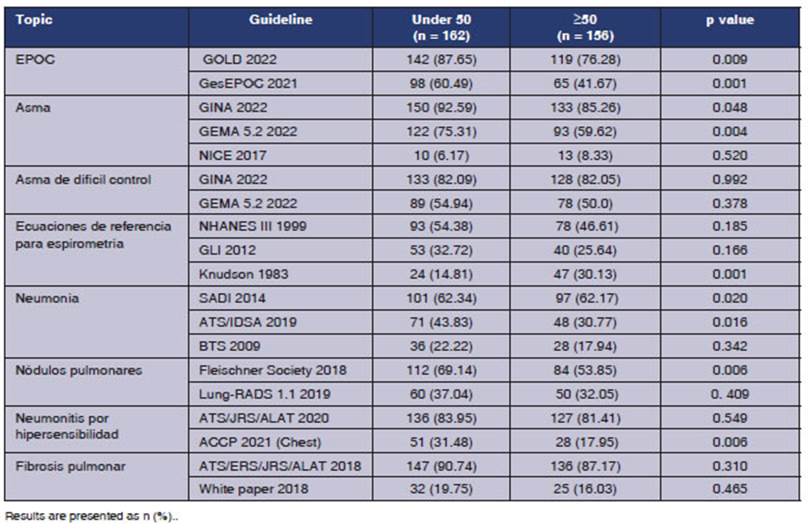
Individuals under the age of 50
reported a staÂtistically significant higher usage of the GOLD and GesEPOC guidelines for COPD, the GINA and GEMA 5.2
guidelines for asthma, the GLI 2012 guideline for spirometry,
the ATS/IDSA 2019 guideline for pneumonia, and the Fleischner
Society 2018 and ACCP 2021 (Chest) guidelines for hypersensitivity pneumonitis
incidental nodÂules. Regarding spirometries, the
group over 50 reported higher use of Knudson’s theoretical reference values.
Table 6 compares the use of
guidelines across groups according to the work environment.
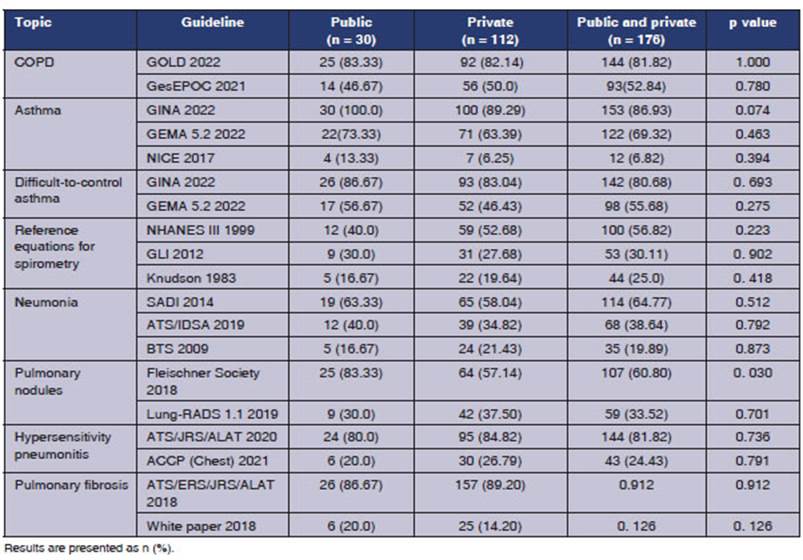
There were no significant
differences in the groups that were divided according to work enviÂronment with
regard to the frequency of use of the guidelines for COPD, asthma, difficult-to-control
asthma, spirometry, pneumonia, hypersensitivity
pneumonitis, or lung fibrosis imaging. Regarding lung nodules, the Fleischner guideline was most frequently used in the public
sector.
DISCUSSION
This research is novel as we have
not found any literature that considers usage preferences among different
guidelines for respiratory diseases in our setting. The diseases under
consideration by the respondents reflect the frequency of these diseases in
consultations to pulmonologists. A study conÂducted in a general population
over 40 years of age from six major regions of Argentina (EPOC.AR), which
included the performance of spirometries, revealed a
prevalence of COPD of 14.5 %.23 Asthma is one of the most prevalent
respiratory diseases in Argentina and worldwide.24 In urban areas of
our country, a telephone survey among individuals aged 20 to 44 identified 5.9
% of 1,521 subjects as asthmatic, while 13.9 % reported having wheezÂing.24
Additionally, it is known that around 5 % of the asthmatic population suffers
from severe forms of this condition.25 Given the need to perform spirometries for the diagnosis and monitoring of these and
other conditions, it was considered inÂteresting to explore whether
pulmonologists used the same equations for their reference values when
reporting them.
There are numerous publications
related to levels of adherence to pulmonology guidelines, many of them in their
early versions. This study addresses another aspect, the preference for one
guideline to another, in the context of Argentina, at a time when many of those
guidelines are well-established and some refer to the same topics, thus
providing the possibility of choice.
In COPD, the GOLD guideline dates
back to 2001, with annual updates and major revisions every 5 years. It is
developed by an international panel of healthcare professionals that includes
experts in respiratory medicine, public health, education, and economics, among
other things.26 Its development responds to
the need for a strateÂgic document to provide effective care for COPD patients
globally. An update from 2023 is availÂable with changes in the classification
and some therapeutic strategies, along with a review of the COVID-COPD
association chapter.27 On the other hand, the first version of the GesEPOC guideline was published in 2012.28 While
not substantially different, the development team of GesEPOC
includes members of the Spanish Patients Forum; it proposes a multidimensional
evaluation, and is one of the first guidelines to conduct treatment acÂcording
to clinical phenotypes.28 The latest updates incorporate the concept
of treatable traits, which would allow for a more personalized approach to
medicine. As for the national guideline from the Ministry of Health, it was
developed in 2017, it has not been updated since then, and has not been widely
disseminated.6 In this study, the GOLD Guideline was reported as the
most commonly used guideline for COPD (82 %), followed by GesEPOC
(51 %); and the least consulted was the one from the Ministry of Health of the
Nation (8 %). In individuals under 50 years, the frequency of use of GOLD and GesEPOC was significantly higher, but there were no
differences according to the proÂfessionals’ work environment. A study
conducted among generalist physicians from two New York hospitals identified
barriers to implementing the GOLD 2010 guideline.29 The difficulties
cited by professionals for not adhering to GOLD guidelines included lack of familiarity,
perceived low benefit, time limitations, and occasionally, disagreement.29
In asthma, the GINA guideline
dates back to 1995, with annual updates since 2002.30 The most recent updates include a significant change in the
management of mild asthma, the first of the five treatment steps, which
relegates short-acting beta 2 agonists (SABAs) to alternative rather than sugÂgested
treatment for exacerbations. The GEMA guideline, whose first edition dates back
to 1997, recognizes six therapeutic steps and, although it allows for combined
treatment with inhaled cortiÂcosteroids, it maintains the use of SABAs as
rescue medication; there is a more detailed breakdown of the treatment for
severe forms in step 6.31 The NICE guideline, of British origin, has
a wide range of recipients (generalist physicians, nurses, proÂfessionals in
secondary and tertiary care services for asthma, patients, and families, among
others) and is organized based on a thematic index.9 The NAEPP
guideline, of American origin, is aimed at professionals and is presented in
the form of quesÂtions, for which answers are given with their level of
evidence and recommendations. 10 It allows for a focused
consultation for a specific problem in the practice. In the present study, the
most reported guidelines were GINA 2022 (89 %) and GEMA 5.2 (68 %), and
respondents under 50 years were the ones who chose them the most. A joint
statement by the ERS and the European Academy of Allergy and Clinical
Immunology (EAACI) warned about suboptimal adherence to these guidelines interÂnationally
and emphasized the need to consider different real-life contexts.32
In difficult-to-control asthma,
GINA 2022 (82 %) and GEMA 2022 (53 %) were mostly used. While
patients are usually assisted in reference centers, respondents report using
the same genÂeral asthma guidelines (GINA and GEMA). There are also
guidelines for difficult-to-control asthma developed by ALAT, which is one of
the societies incorporated into the GEMA guidelines, that is why they were not
specifically consulted in this survey.33
Regarding reference equations for
spirometry, the use of one or the other can affect
the diagnosis of airway obstruction and the estimation of its seÂverity.34
One of the oldest, the Knudson equation, was based on a North American white
population; 746 patients aged 8 to 90, and emerged to detect diseases in
textile workers due to cotton expoÂsure.35 It was later expanded to
include African Americans but not Latin Americans. In 2005, the ATS and ERS
recommended the use of the equaÂtion known as NAHNES III for US patients aged
between 8 and 80 years.34 In order to extend the reference to other
groups, the GLI 2012 included 57,395 Caucasians, 3,545 African Americans, and
13,247 Asians; the age range extended from 3 to 95 years.12 These
last two equations have shown good correlation with each other for average
adults, which is not the case when dealing with patients older than 80 years,
particularly those of extreme heights (very short or very tall).34 A
study conducted in Chile included the comparison of the Knudson equation (the
most commonly used by laboratories in that country) with the Gutiérrez 2014
equation (designed for the Chilean populaÂtion) and GLI 2012, in 315 subjects
over 40 years, smokers or ex-smokers, healthy or with COPD, and found good
correlation between the three.36 It has been suggested that the
Knudson equation underestimates restriction compared to NHANES III.36
In Argentina, functional measurements were performed on 105 women and 132 men
from the Capital City and Metropolitan Area of Buenos AiÂres, between 18 and 86
years old, and the Lower Limit of Normality (LLN) was determined as a variable
percentage for each parameter, at each age, and at each height, thus
eliminating the concept of a fixed percentage value, which led to underdiagnosis in younger individuals and overÂdiagnosis in older ones.37 In Mendoza, a
similar study was carried out on 103 healthy volunteers, aged 15 to 65 years,
who underwent spirometry, and a smaller number
underwent peak expiratory flow, measurements of mean inspiratory and expiÂratory
pressures (MIP and MEP), and a 6-minute walk test.38 Good
correlation was found between NHANES and the Mendoza sample, especially in spirometric values, except for the FEV1/FVC ratio (forced
expiratory volume in the first second/forced vital capacity) where the LLN was
a better option for defining normality.38
In our work, the most commonly
used equation was NHANES III, which may be related to the fact that most spirometry equipment has it incorÂporated into their
software. The increased use of the GLI equation among young people could be
explained by the fact that it includes multiethnic groups, has a wider age
range (3 to 95 years), and was gradually included in new equipment.12
ConÂversely, the use of the Knudson equation, which is used by one-fifth of the
respondents, predominates among those over 50 years and may be attributed to
the age of the equipment or to the lesser flexibilÂity in adapting to changes
found in this age group.
In pneumonia, the national
guideline of SADI was the most commonly used among our responÂdents, despite
not being updated since 2014. This is attributed to the fact that, it being an
infecÂtious disease, local epidemiological factors and available antibiotics in
our country are taken into account as well as being more user-friendly due to
its concise nature and for being in the Spanish language. Gatarello
et al studied the adherence of respondents to the IDSA/ATS pneumonia guideÂline
and included 36 Latin American physicians.39
Treatment was considered appropriate in 30.6 % of prescriptions for
community-acquired pneumonia. The use of antibiotics with inadequate
spectrum, monotherapy, or coverage not indicated for
multiÂdrug-resistant organisms was considered as lack of adherence. In the case
of nosocomial pneumonia, compliance with the IDSA/ATS guidelines was only 2.8 %
(monotherapy and lack of dual antibiotic treatment
against Pseudomonas aeruginosa).39
Regarding pulmonary nodules, the
most freÂquently chosen guideline was the Fleischner
Society 2018, which was developed for the manÂagement of incidental nodules,
that is to say, those appearing during a chest CT scan for any requested
reason.17 Its goal is to limit further evaluations of nodules with
very low probability of cancer (<1 %) and not overlook them if the
probability is ≥1 %.17 Hedstrom et
al studied the adherence of radiologists and clinicians to the Fleischner Society guidelines with regard to the management
of incidental lung nodules and found that around 5 % conducted a more
aggressive follow-up and in 9 % of the cases, the follow-up was less aggressive
than recommended.40 In contrast, Lung-RADS is oriented towards the management
of nodules found during screening, corresponding to indiÂviduals with
sufficient risk to qualify for these programs.18 Moreover, the
number of centers curÂrently conducting screening in our country is not high,
hence the lower familiarity with Lung-RADS.
When analyzing guidelines for
hypersensitivity pneumonitis, a clear preference is observed for the 2020
ATS/JRS/ALAT guidelines. Its dissemination during the pandemic and its temporal
precedence over the ACCP guidelines could explain this choice. Among those who
chose the ACCP guidelines, the ones under 50 years prevailed. As already menÂtioned, the study protocol allowed for opting for
more than one guideline, according to the needs.
With regard to the images
supporting the diagÂnosis of pulmonary fibrosis, the use of ALAT/ERS/ JRS was
predominant, and this can be attributed to its wider dissemination and the fact
of havÂing been elaborated by multiple societies, which provides more
robustness. However, there are no major differences between these guidelines
and the Fleischer Society White paper. Both identify key questions and provide
radiological and tissue images that are prototypical of each proposed category.
The latter adds a checklist at the end to rule out alternative diagnoses.
Several authors of
hypersensitivity pneumonitis and pulmonary fibrosis guidelines warn in a recent
publication that, as each guideline is developed independently, they do not
reflect the physician’s needs when faced with a patient who does not yet have a
diagnosis and is within a spectrum of fiÂbrotic diseases that may include both
conditions.43 With a pragmatic approach, they suggest using an
algorithm that integrates these two guidelines and includes both clinical,
radiological, and pathologiÂcal features to distinguish hypersensitivity
pneumonitis from pulmonary fibrosis.41
In general terms, although
respondents were not asked to justify their choice, it can be specuÂlated that
professionals’ preference for different guidelines is due to the fact that they
were origiÂnated from well-known societies, which respond to a rigorous and
updated review of the best available scientific evidence. In the case of the
Argentine guideline on pneumonia, the local relevance of the recommendations is
privileged. Another factor that may determine the choice is the availability of
the equipment or supplies suggested in the stanÂdards, because if they are not
available, the guideÂline is less applicable. Finally, once professionals
become familiar with one particular guideline and have experience with it, they
incorporate updates more naturally.
This study acknowledges
limitations, mainly the number of respondents, given that only 33 % of those
who received the survey responded. It was conducted among pulmonology
specialists from the AAMR, excluding other specialties or pulmonoloÂgists not
associated. There is also the limitation of having omitted some guidelines that
are possibly used. Recently, the ERS/ESICM (European Society of Intensive care
Medicine)/ESCMID (European Society of Clinical Microbiology and Infectious
Diseases)/ALAT have released a guideline for the management of severe
community-acquired pneuÂmonia, which has not been part of our survey.42
However, their results allow us
to explore the current reality regarding the use of the guidelines and make
some general recommendations. The need to use updated guidelines is emphasized,
as this improves the quality of care, increases patient safety, provides legal
and juridical support for professionals, and optimizes cost-effectiveness.
Scientific societies together with national health authorities should encourage
guideline update and availability. Likewise, treatments proposed with strong
evidence should be available in the country, avoiding dissociation between
recommendations and daily practice. Referring specifically to one of the
guidelines subjected to the survey in this research, we suggest that the GLI spirometric reference equation is used in our equipment,
for the advantages mentioned before. Similarly, it would be of high priority to
update the national guideline for acute community-acquired pneumoÂnia, with the
participation of all societies involved in its management.
In conclusion, an analysis of the
situation has been described as of the end of 2022 regarding the use of
guidelines for prevalent respiratory diseases by a group of 318 pulmonologists
who are members of the AAMR. Although there is a trend among respondents under
50 to use the most recent guidelines, the use of updates from long-standing
guidelines of the main scientific societies in the specialty, such as GOLD in
COPD, GINA in asthma, and SADI in pneumonia, remains very strong in all groups.
Acknowledgement
To the authorities of
the AAMR, to the secretaries of the AAMR, and the webmaster Muriel Cabrera.
Conflict of interest
The authors have no conflict of
interest to declare that are relevant to this publication.
REFERENCES
1. Soler-Cataluña
JJ. Clinical practice guidelines or personalÂized medicine in
chronic obstructive pulmonary disease? Arch Bronconeumol (Engl Ed).
2018;54:247-8. https://doi.org/10.1016/j.arbres.2017.08.002
2. Goldberger JJ, Buxton AE. Personalized medicine vs guideÂline-based
medicine. JAMA.
2013;309:2559-60.
https://doi.org/10.1001/jama.2013.6629.
3.
Grupo de trabajo para la actualizaciĂłn del Manual de ElaboÂraciĂłn de GPC.
ElaboraciĂłn de GuĂas de Práctica ClĂnica en el Sistema Nacional de Salud.
ActualizaciĂłn del Manual MetodolĂłgico [Internet]. Madrid: Ministerio de
Sanidad, Servicios Sociales e Igualdad; Zaragoza: Instituto Aragonés de
Ciencias de la Salud (IACS); 2016. Disponible en: http://portal.guiasalud.es/emanuales/elaboracion_2/?capitulo.
4. Venkatesan P. GOLD report:
2022 update. Lancet Respir Med. 2022;10: e20.
https://doi.org/10.1016/S2213-2600(21)00561-0.
5.
Miravitlles M, Calle M, Molina J, et al. Spanish COPD Guidelines (GesEPOC)
2021 Updated PharmacologiÂcal treatment of stable COPD. Arch Bronconeumol. 2022;58:69-81. https://doi.org/10.1016/j.arbres.2021.03.005
6.
Argentina. Ministerio de Salud de la NaciĂłn. GuĂa breve de EPOC. —1a ed.— Ciudad AutĂłnoma de Buenos Aires: Ministerio de Salud de
la NaciĂłn, 2017. 40p.
7. Global Initiative for Asthma. Global strategy for asthma management and prevention. 2022. Disponible en:
www.ginasthma.org
8.
Sociedad Española de NeumologĂa y CirugĂa Torácica. GEMA 5.2 GuĂa Española para
el manejo del asma. 2022. Disponible
en: www.gemasma.com
9. National Institute for Health
and Care Excellence (NICE). Asthma: diagnosis, monitoring and chronic asthma
manÂagement. London; 2021 Mar 22. PMID: 32755129. Nice 2017
10. National Asthma Education and
Prevention Program. Expert Panel Report: Guidelines for the Diagnosis and
Management of Asthma. Bethesda, Maryland: National Heart, Lung, and Blood
Institute, National Institutes of Health. 2020.
11. Hankinson JL, Odencrantz JR, Fedan KB. Spirometric reference values from a sample of
the general U.S. populaÂtion. Am J Respir Crit Care Med. 1999;159:179-87.
https://doi.org/10.1164/ajrccm.159.1.9712108.
12. Quanjer
PH, Stanojevic S, Cole TJ, et al; ERS Global Lung
Function Initiative. Multi-ethnic reference values for spiÂrometry
for the 3-95-yr age range: the global lung function 2012 equations. Eur Respir J. 2012;40:1324-43. https://doi.org/10.1183/09031936.00080312.
13. Knudson RJ, Lebowitz MD, Holdberg CJ, Burrows
B. Changes in normal maximal expiratory flow-volume curve with growth and
aging. Changes in the normal maximal expiratory flow-volume curve with growth
and aging. Am
Rev Respir Dis. 1983;127:725-34.
14.
Lopardo G, BasombrĂo A,
Clara L, Desse J, De Vedia
L, Di Libero E, et al. NeumonĂa adquirida de la comunidad en adultos.
Recomendaciones sobre su atenciĂłn. Medicina (Buenos Aires). 2015;75:245-57.
15. Metlay
JP, Waterer GW, Long AC, et al. Diagnosis and TreatÂment
of Adults with Community-acquired Pneumonia. An Official
Clinical Practice Guideline of the American ThoÂracic Society and Infectious
Diseases Society of America. Am J Respir Crit Care Med. 2019; 200:e45-e67.
https://doi.org/10.1164/rccm.201908-1581ST.
16. Lim WS, Baudouin
SV, George RC, et al. Pneumonia GuideÂlines Committee of the BTS Standards of
Care Committee. BTS guidelines for the management of community acquired
pneumonia in adults: update 2009. Thorax. 2009;64 Suppl 3:iii1-55.
https://doi.org/10.1136/thx.2009.121434.
17. Bueno
J, Landeras L, Chung JH. Updated Fleischner Society Guidelines for Managing Incidental
Pulmonary Nodules: Common Questions and Challenging Scenarios. Radiographics.
2018;38:1337-50.
https://doi.org/10.1136/thx.2009.121434
18. ACoR.
ACR Lung-RADS - Update 1.1 2019. 2019. DisÂponible en:
https://www.acr.org/-/media/ACR/Files/RADS/Lung-RADS/LungRADS-1-1-updates.pdf?la=en.
https://doi.org/10.1148/rg.2018180017
19. Raghu G, Remy-Jardin M, Ryerson CJ, et al. Diagnosis of Hypersensitivity
Pneumonitis in Adults. An Official ATS/ JRS/ALAT Clinical
Practice Guideline. Am J Respir Crit Care Med. 2020;202(3):
e36-e69. https://doi.org/10.1164/rccm.202005-2032ST.
20. Fernández
PĂ©rez ER, Travis WD, Lynch DA, Brown KK, Johannson
KA, Selman M, et al. Diagnosis and Evaluation of Hypersensitivity Pneumonitis:
CHEST Guideline and Expert Panel Report. Chest. 2021;160(2):e97-e156.
https://doi.org/10.1016/j.chest.2021.03.066.
21. Raghu G, Remy-Jardin M, Myers JL, et al. American Thoracic Society,
European Respiratory Society, JapaÂnese Respiratory Society, and Latin American
Thoracic Society. Diagnosis of Idiopathic Pulmonary Fibrosis.
An Official ATS/ERS/JRS/ALAT Clinical Practice Guideline.
Am J Respir Crit Care Med.
2018;198:e44-e68.
https://doi.org/10.1164/rccm.201807-1255ST.
22. Lynch DA, Sverzellati
N, Travis WD, et al. Diagnostic criteÂria for idiopathic pulmonary fibrosis: a Fleischner Society White Paper. Lancet Respir
Med. 2018;6:138-53.
https://doi.org/10.1016/S2213-2600(17)30433-2.
23.
Echazarreta AL, Arias SJ, Del Olmo R, et al; Grupo de
estudio EPOC.AR. Prevalencia de enfermedad pulmoÂnar obstructiva crĂłnica en 6
aglomerados urbanos de Argentina: el estudio EPOC.AR. Arch
Bronconeumol (Engl Ed).
2018;54:260-9. https://doi.org/10.1016/j.
arbres.2017.09.018.
24. Arias SJ, Neffen
H, Bossio JC, et al. Prevalence and FeaÂtures of
Asthma in Young Adults in Urban Areas of ArgenÂtina. Arch Bronconeumol (Engl Ed).
2018 Mar;54(3):134-9.
https://doi.org/10.1016/j.arbres.2017.08.021.
25. Shah PA, Brightling
C. Biologics for severe asthma-Which, when and why? Respirology. 2023;28:709-21. https://doi.org/10.1111/resp.14520.
26. Mirza
S, Clay RD, Koslow MA, Scanlon PD. COPD Guidelines: A
Review of the 2018 GOLD Report. Mayo Clin Proc. 2018;93:1488-502. https://doi.org/10.1016/j.mayocp.2018.05.026.
27. Global Initiative for Chronic
Obstructive Lung Disease (GOLD), Global strategy for the diagnosis, management,
and prevention of chronic obstructive lung disease (2023 Report).
https://goldcopd.org/2023-gold-report-2/
28.
Miravitlles M, Soler-Cataluña JJ, Calle M, et al.
GuĂa Española de la EPOC (GesEPOC).
Tratamiento farmaÂcolĂłgico de la EPOC estable [Spanish
COPD Guidelines (GesEPOC): Pharmacological treatment of stable COPD]. Aten Primaria. 2012;44:425-37.
https://doi.org/10.1016/j.aprim.2012.04.005.
29.
PĂ©rez X, Wisnivesky JP, Lurslurchachai
L, Kleinman LC, Kronish IM.
Barriers to adherence to COPD guidelines among primary
care providers. Respir Med. 2012;106:374-
81. https://doi.org/10.1016/j.rmed.2011.09.010.
30. Bateman ED, Hurd SS, Barnes PJ, et al. Global strategy for asthma
management and prevention: GINA execuÂtive summary. Eur Respir J.
2008;31:143-78. https://doi.org/10.1183/09031936.00138707.
31.
Hidalgo PP. Asma: GINA 2022 vs Gema 5.2. Respiratorio en AtenciĂłn Primaria No.
2. Revista online disponible en:
https://www.livemed.in/canales/respiratorio-en-la-red/respiratorio-atencion-primaria/numero-2/asma-gina-2022-gema-5-2.html#:~:text=Tanto%20la%20GINA%20(Global%20Initiative,la%20gu%C3%ADa%20GEMA%20es%20espa%C3
%B1ola
32. Mathioudakis
AG, Tsilochristou O, Adcock IM, et al. ERS/ EAACI
statement on adherence to international adult asthma guidelines. Eur Respir
Rev. 2021;30:210132.
https://doi.org/10.1183/16000617.0132-2021.
33.
GarcĂa G, Bergna M, Vásquez JC, et al. Severe asthma: adding new evidence - Latin American Thoracic SoÂciety.
ERJ Open Res. 2021;7:00318-2020.
https://doi.org/10.1183/23120541.00318-2020.
34. Linares-Perdomo
O, Hegewald M, Collingridge
DS, et al. Comparison of NHANES III and ERS/GLI 12 for airway obstruction
classification and severity. Eur Respir
J. 2016;48:133-41.
https://doi.org/10.1183/13993003.01711-2015.
35. LĂłpez
A, Benavides-Cordoba V, Palacios M. Effects of changÂing reference values on
the interpretation of spirometry for rubber workers. Toxicol Rep. 2023;10:686-9. https://doi.org/10.1016/j.toxrep.2023.05.011.
36.
Dreyse J, Gil R. Ecuaciones de referencia para
informe de espirometrĂas. ÂżSerá tiempo de adoptar las
ecuaciones de la Global Initiative for Lung Function?
Rev Chil Enferm Respir. 2020;36: 13-7. https://doi.org/10.4067/S0717-73482020000100013
37.
GalĂndez F, SĂvori M,
GarcĂa O, et al. Valores espiromĂ©triÂcos normales
para la Ciudad de Buenos Aires. Medicina (Buenos Aires) 1998;58:141-6.
38.
Lisanti R, Gatica D, Abal
J, et al. ComparaciĂłn de las prueÂbas de funciĂłn pulmonar en poblaciĂłn adulta
sana de la Provincia de Mendoza, Argentina, con valores de referencia
internacionales. Rev Am Med
Respir 2014;14:10-9.
39.
Gattarello S, RamĂrez S, Almarales
JR, Borgatta B, LaÂgunes L,
Encina B, Rello J; investigadores del CRIPS. Causes of non-adherence to therapeutic guidelines in
severe community-acquired pneumonia. Rev Bras Ter Intensiva.
2015;27:44-50.
https://doi.org/10.5935/0103-507X.20150008.
40. Hedstrom
GH, Hooker ER, Howard M, et al. The Chain of Adherence for Incidentally
Detected PulÂmonary Nodules after an Initial Radiologic Imaging Study: A
Multisystem Observational Study. Ann Am Thorac Soc.
2022;19:1379-89.
https://doi.org/10.1513/AnnalsATS.202111-1220OC.
41. Marinescu
DC, Raghu G, Remy-Jardin M, et al. Integration and
Application of Clinical Practice Guidelines for the Diagnosis of Idiopathic
Pulmonary Fibrosis and Fibrotic Hypersensitivity Pneumonitis. Chest. 2022;162:614-29.
https://doi.org/10.1016/j.chest.2022.06.013.
42. Martin-Loeches
I, Torres A, Nagavci B, et al. ERS/ESÂICM/ESCMID/ALAT
guidelines for the management of severe community-acquired pneumonia. Eur
Respir J. 2023;61:2200735. https://doi.org/10.1183/13993003.00735-2022