Autor :Torres, RubĂ©n1, Masdeu, MartĂn1, Meza, Adriana1, MorĂłn, Karen1, Vespa, Franco1, Codinardo, Carlos1
1Pulmonology Section, Department of Medicine, Hospital Pirovano, Buenos Aires, Argentina
https://doi.org/10.56538/ramr.YJNV3347
Correspondencia : Rubén Torres. E-mail: rubencildo79@gmail.com
ABSTRACT
The control of oxygen saturation
during hospital admission is a daily challenge for the treating physician,
whether in the context of a COPD exacerbation or any acute disease that occurs
with respiratory failure. The adjustment of the oxygen flow administered to the
patient is mostly manual, usually without a clear medical prescription for the
desired SpO2 range,
implying an overload of the nursing service with the risk of making an inÂadequate
contribution, either over-administering it or providing it incorrectly. insufficient. The objective of this work is to describe a
preliminary experience with the automated administration of the O2 flow through
the use of the O2matic
device. A group of adult patients with acute respiratory failure who were
hospitalized using continuous oxygen therapy with conventional flowmeters and periodic nursing manual controls was
studied, after which it was indicated to start oxygen therapy in a controlled
manner using the O2matic
device for 30 minutes. It was observed that the oxygen flow achieved using the
O2matic
automatic control device has been lower than the flow used in manual control,
with significant differences between both values found, with adequate safety and
patient tolerance. Whether the automation of oxygen therapy during hospital
admission could reduce the length of admission, and possibly improve survival
among patients with acute respiratory failure remains to be determined,
requiring future randomized studies with a larger sample of patients.
Key words: Oxygen Inhalation Therapy, Respiratory Insufficiency
RESUMEN
El
control de la saturaciĂłn de oxĂgeno durante el ingreso hospitalario es un
desafĂo cotidiano para el mĂ©dico tratante, ya sea en contexto de una
exacerbaciĂłn de EPOC o cualquier enfermedad aguda que curse con insuficiencia
respiratoria. El ajuste de flujo del oxĂgeno administrado al paciente es en la
mayorĂa de los casos manual, habitualÂmente sin una prescripciĂłn mĂ©dica clara
del rango de SpO2 deseado, lo
que implica una sobrecarga del servicio de enfermerĂa con el riesgo de realizar
un aporte inadecÂuado de este, ya sea por sobreadministraciĂłn
o por aporte insuficiente. El presente trabajo tiene como objetivo describir
una experiencia preliminar con la administraciĂłn automatizada del flujo de O2 mediante el
uso del dispositivo O2matic.
Se estudiĂł un grupo de pacientes adultos con insuficiencia respiratoria aguda
quienes se encontraban internados usando oxigenoterapia continua con flujĂmetros convencionales y controles manuales periĂłdicos
de enfermerĂa, por lo que se indica, luego, iniciar oxigenoterapia en forma
controlada usando el dispositivo O2matic
durante 30 min. Se ha observado que el flujo de oxĂgeno alcanzado utilizando el
dispositivo de control automático O2matic
ha sido menor al flujo utilizado en el control manual, con diferencias
significativas entre ambos valores hallados, con adecuada seguridad y
tolerancia del paciente. Que la automatizaciĂłn de la oxigenoterapia durante el
ingreso hospitalario pueda reducir la duraciĂłn de la admisiĂłn, y posiblemente
mejorar la supervivencia entre pacientes con insuficiencia respiratoria aguda
queda aĂşn por determinar, por lo que son necesarios futuros estudios
aleatorizados con una muestra mayor de pacientes.
Palabras
clave: Terapia
por InhalaciĂłn de OxĂgeno, Insuficiencia Respiratoria
Received: 23/12/2022
Accepted: 15/06/2023
INTRODUCTION
Treatment with supplementary oxygen
is essential for the proper management of hospitalized paÂtients suffering from
hypoxemic acute respiratory failure (ARF) or worsening of chronic respiratory
failure. Like other drugs, medical oxygen is a gaseous medication that should
be administered with previously titrated doses or previously speciÂfied oxygen
flow values. Since the last century, the administration of medical oxygen flow
has been controlled through flowmeters with a
manually adjustable scale in order to correct hypoxemia. Following verbal or
written medical instructions, the nursing staff manually adjusts the value to
achieve an acceptable saturation, recommended to be between 88 % and 92 % if
there is suspicion of hypercapnia, or between 92 % and 96 % if there is no such risk or suspicion.
This is suggested by several specific published international guidelines on the
treatment of acute hypoxemic respiratory failure.1-3
Supplementary oxygen is often
administered generously and freely to patients with respiratory failure, a
methodology that has been used worldÂwide for over 100 years.
In recent years, automated
devices have been available in other countries (models FreeO2
from the OxyNov company in Canada and O2matic
from the O2matic
company in Denmark), with clear benefits demonstrated in clinical trials.4-6
The purpose of this preliminary
study has been to examine the ability of the O2matic device to maintain the SpO2 of patients
with ARF within a prespecified target interval. The findings
were compared with the previous manual control of oxygen flow in the same
patient, and the patient’ s perception and sense of
safety regarding autoÂmated oxygen control were evaluated.
METHODOLOGY AND STUDY DESIGN
This is a descriptive study in
which, in November 2022, we recruited a group of hospitalized adult patients
with acute respiratory failure who were using continuous oxygen therapy with
convenÂtional flowmeters, with periodic manual
control by nursing staff. Five (5) patients were recruited and entered the
study in a descriptive design of oxygen use. The study was authorized by the
Ethics Committee of the Hospital Dr. I Pirovano,
without obtaining informed consent from the selected patients.
Device or equipment used (O2matic)
The O2matic oxygen therapy device is an electronic equipment that complies with the CE standards
and is currently authorized for use in hospitals in several European countries.
It has an electronic closed-loop system that, based on continuous moniÂtoring
of heart rate and SpO2 by a standard
wired pulse oximeter, adjusts oxygen flow to the
patient (Figure 1). The algorithm in O2matic allows it to calculate increments
or decrements in oxygen flow based on the last 15 seconds sensed by the pulse oximeter. Increments and decrements change proportionally
in relation to the difference between the actual SpO2
and the prespecified target SpO2. The
oxygen flow can be specified to fit the actual condition and the device used
for delivering oxygen to the patient (nasal cannula). O2matic allows for flow up to 15 L/minute
in automatic mode, but in the original study, most patients received an
acceptable flow range from 0 to 8 L/minute with a standard nasal cannula. If
minimal prespecified SpO2
cannot be maintained with the maximal oxygen flow allowed, an
alarm will sound that will intensify if SpO2
drops 0.3 % below the target interval or below 85 %. The alarms
will also be visible and audible and activate if the heart rate is outside the
range defined by the user.

Patients
Adult patients recruited for the
study showed acute respiratory failure with minimum previous hospitalization
for 48 hours. Inclusion required a PaO2
of less than 60 mmHg or SpO2
of up to 88 %, on room air. Patients were excluded if they were hemodynamically unstable or had an impaired level of
consciousness. Patients deemed at high risk for need of mechanical ventilation
were not included in the study.
Study intervention
Enrolled patients were receiving
oxygen under “manual control”, using a conventional manual ball flowmeter. Thus, SpO2
and pulse rate were measured at baseline with another pulse oximeter (model NONIN 8500) in order to adjust oxygen
supply. Then it was indicated to initiate oxygen therapy in a controlled
fashion using the O2matic
device for 30 minutes (Figure 2). Allocation to the sequence was consecutive in
each patient, with no defined randomization.

Previously, the corresponding
mode was selected in the device, with SpO2
target range set between 92 %-96 % and oxygen flow between 0 and
8 L/ minute. Patients were monitored for SpO2, oxygen flow, heart rate and other
data. All events during the 30-minute period were managed by personnel assigned
to the study. The patient was instructed to lie in bed during the study. Oxygen
flow was delivered without humidification by standard nasal cannula.
RESULTS
Eight (8) patients were
considered as candidates, and five (5) of them were selected. Three patients
were unable to participate due to difficulties in connecting the regulator to
the wall oxygen outlet; 4 patients (80 %) had acute community-acquired
pneumonia. At inclusion, the mean baseline SpO2
was 87.8 % with an average supplemental oxygen flow of 3
liters/minute, and the flow range on the device was set between 0 and 8 liters
/minute. See Table 1.
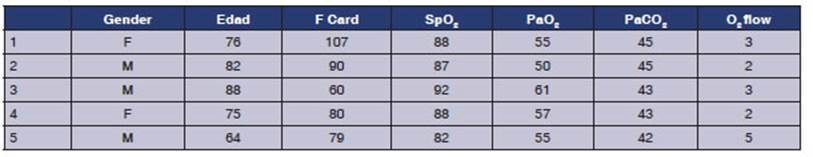
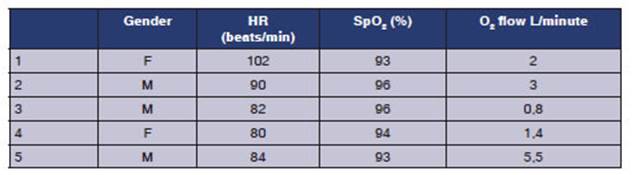
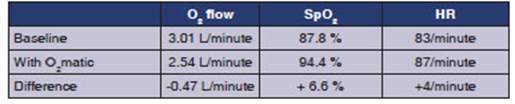
On average, patients received
oxygen with O2matic
in automatic mode for 30 minutes comÂpared to 30 minutes in the previous manual
mode (P=XX). Mean oxygen flow was 2.54 liters/minute in automatic mode and 3
liters/minute in baseline manual control mode (P=0.05). Mean heart rate was
similar in the two periods (83.2/minute for baseline vs. 87.6/minute under
automatic control P=XX). See Table 3.
Primary outcome
We have observed that the oxygen
flow rate achieved using the O2matic
automatic control deÂvice was lower than the one achieved with manual control,
with significant differences between both values. See Table 3.
The target interval in the SpO2 device was beÂtween
92 % and 96 %, for all analyzed patients, as can be seen in Table 3. Comparison of SpO2 before and
after using O2matic.
Secondary outcomes
Subjective tolerance to the use
of the device was adequate and expressed by all patients, with no references of
dyspnea symptoms or discomfort related to the use of oxygen therapy. To collect
this information, simple questions were asked, not based on a previously
validated questionÂnaire.
Safety of use of the device
In one case, audible and visible
alarms for lack of power supply and low battery were ignored, resultÂing in the
need to connect the device to AC power (in accordance with battery life
specifications in O2matic).
No other safety issues were observed. The battery of the device allows for
stand-alone use without connection to power supply for 4 (four) hours.
Other outcomes
Data could be analyzed from the 5
(five) patients who completed the study out of the 8 (eight) candidate
patients. None of the patients showed specific symptoms related to the use of
the device, with confidence proportional to the use of oxygen through the
conventional nasal cannula used.
Two patients showed
some limitation of moveÂment caused by the pulse oximeter
cable. All patients felt confident using the device. On two occasions,
difficulty was noted in attaching the device to the wall’s medical gas outlet polyduct due to missing fasteners. Unfortunately, this
difficulty had not been evaluated prior to the study.
In general, the sense
of safety was very strong with the automated oxygen concept, although this was
a subjective impression of the investigators on an observational basis.
DISCUSSION
The observed data have
allowed us to say that automated control of oxygen supply to the patient is
reliable, feasible and superior to manual control in the use of oxygen therapy,
to make it possible for the SpO2 to reach the target prescribed by
the treating physician.
Although
oxygen flow has been lower when using automated flow control, no significant
difÂference in medical oxygen consumption could be demonstrated with O2matic
compared to manual control.
The mean oxygen flow was 2.54 L/minÂute using O2matic and 3 L/minute
with manual control. We believe that the limited number of patients does not
allow us to infer a lower oxygen consumption, although
our study was not powered to study this result. In the two cited studies with
the use of FreeO2, there was a reduction in oxygen consumption from
1.2 L/minute to 0.7 L/minute (P=0.06), and no overall difference was observed
in another study where the average flow was 4.6 L/minute with FreeO2
and 4.2 L/minute with manual control.5,6
However, the trend
observed in our study toÂward higher flow with manual control compared to O2matic
is consistent with such findings in the literature.
Medical prescribing
practices for oxygen use in patients with ARF are limited and reflect a lack of
awareness of the need for accurate oxygen prescription and therapy.3,7
A 2013 audit by the British Thoracic Society found that only 55 % of patients
who had received oxygen during hospiÂtalization had a written prescription.
However, this has improved since 2008, where only 32 % of patients supplied with
oxygen had had it preÂscribed in written form.8 In an audit carried
out in Australia, only 3 % of patients hospitalized with a COPD exacerbation
had a written oxygen prescription regardless of the fact that 79 % of patients
required oxygen supplements.8 A large European retrospective study
conducted an audit in 2011 of 16,018 patients with a COPD exacerbaÂtion, and
found that 10.1 % received inadequate treatment with oxygen therapy, either
with high-flow oxygen or no oxygen at all, despite having hypoxemia.9
Patient acceptance of
automated oxygen adÂministration in our study was very high, and in general,
patients were highly confident that they were receiving oxygen in an adequate
manner. However, limitation of movement due to the pulse oximeter
cable has been a problem for some patients. As our study was limited to 30
minutes of continuous SpO2 monitoring during the day, prolonged
studies including overnight would be necessary to adequately assess the
individual patient experience with continuous monitoring under automated oxygen
flow control. Our work is a preliminary and descriptive study and, therefore,
did not allow the examination of certain outcomes such as time to oxygen
weaning and overall duraÂtion of hospitalization, which would have been valuable
to understand the real value of these new technologies.
A retrospective study
of 680 patients with COPD exacerbation showed that SpO2 control
during hospital admission is a time-consuming task for the nursing staff,
considering that closed-loop control of oxygenation could reduce their workload
and increase patient safety through better SpO2 control.
In another study
controlled by a closed-loop system, FreeO2®, OxyNov Inc., Quebec, Canada, an increase in time with
target SpO2 was observed between 51 % and 81 % compared to manual
control.6 Results for FreeO2 were confirmed in a shorter
3-hour study of 187 patients with hypoxÂemic respiratory failure due to
different conditions in the emergency room.3,6
Other studies have
shown that closed-loop control of oxygen probably allows for faster oxyÂgen
weaning and shorter hospital length of stay; therefore, it could be beneficial
to the management of resources, in comparison with manual control by the
nursing staff.5,6 The automatic adjustment
of oxygen flow would optimize the use of this reÂsource that is frequently
over-administered when flow control is manual, as it has already been
mentioned.
These findings
inspire us to carry out a comÂparative study between 2 (two) groups of
patients, one under manual control of oxygen therapy by a conventional flowmeter, and another group using O2matic
permanently for at least 24 to 48 hours, in a number of patients of at least 3
digits, so as to be able to evaluate differences in real nursing working time,
in the patient’s number of hospitalization days, and total time in hypoxemia
under oxygen therapy, among other objectives.
A relevant issue is
the clinical importance of keeping the SpO2 within a fairly narrow
interÂval. Controlled studies of outcome in terms of prescription and adherence
to different oxygen dosing regimens are still necessary, for example, for
patients with an exacerbation of COPD. Thus, either a disproportionately
elevated or decreased SpO2 on admission has been associated with
worse outcomes in terms of mortality or other serious adverse effects.4,5 It seems reasonable to assume that findings from
studies at the pre-hospital and admission level can be extrapolated to similar
conÂditions during hospitalization, but further studies are needed to evaluate
the outcomes related to episodes of prolonged hypoxemia and hyperoxia.
We were unable to
evaluate the effect of the closed-loop oxygen control on arterial pressure of
CO2 (PaCO2) in our study. It is well known that an
increase in arterial pressure of oxygen can increase PaCO2 as a
consequence of the Haldane effect and increased dead space ventilation caused
by the reversing of pulmonary vasoconstriction due to hypoxemia and worsening
of ventilation-perfusion inequality.3,10
However, the recommended strategy to avoid CO2 retention is to avoid
hyperoxia and control SpO2 between 88 %
and 92 %.2 This makes CO2 retention more unlikely when SpO2
is better controlled.
This study describes preliminary
data on the clinical use of an automated oxygen administration control device
(O2matic device) in patients hospiÂtalized with respiratory failure in general
wards of a University Hospital in Buenos Aires, Argentina.
CONCLUSION
In a limited number
of patients with acute respiÂratory failure, we have observed that this device
(O2matic) allows for the optimization of the autoÂmatic control of
SpO2 in hospitalized patients with respiratory failure, and we can
describe some of the benefits observed.
The use of O2matic
has been more effective than conventional manual control in maintaining the
patient’s SpO2 within the specified target interval. Patients
accepted the automatic oxygen control well and felt confident about getting the
right amount of oxygen.
The possibility to
analyze the effect of autoÂmated oxygen flow control on the duration of the
patient’s hospital length of stay and the actual time spent by the nursing
staff to manually correct the flow, optimizing hidden factors in the management
and handling of oxygen therapy during hospitalizaÂtion remains to be determined
in a study with a larger number of patients.
In conclusion, the
question of whether the automation of oxygen therapy during hospital admission
can reduce the duration of admission, and possibly improve survival among
patients with acute respiratory failure remains to be determined.
We are grateful for
the collaboration of the Linde-Praxair Company of
Argentina, for proÂviding an O2matic device and for the training in the use and
control of data collection by Engineer RocĂo SantamarĂa, manager of said Company.
REFERENCES
1. Global Initiative
for Chronic Obstructive Lung Disease. Global strategy for the
diagnosis, management and preÂvention of COPD; 2018. Available from:
https://goldcopd.org/wp-content/uploads/2017/11/GOLD-2018-v6.0-FINAL-revised-20-Nov_WMS.pdf.
Accessed December 02, 2018.
2. British Thoracic
Society Emergency Oxygen Guideline Development Group. BTS
guideline for oxygen use in adults in healthcare and emergency settings.
Thorax. 2017;72:i1- i90.
https://doi.org/10.1136/thoraxjnl-2016-209729
3. Codinardo y cols. Oxigenoterapia:
Usos mĂ©dicos en situaÂciones agudas y crĂłnicas. EdiciĂłn 2020.Editorial Journal.
4. Hansen EF, Hove
JD, Bech CS, Jensen JS, Kallemose
T, Vestbo J. Automated oxygen control with O2matic®
during admission with exacerbation of COPD. Int J Chron Obstruct Pulmon Dis. 2018;13:3997-4003. https://doi.org/10.2147/COPD.S183762
5. Lellouche F, Bouchard PA, Roberge
M, et al. Automated oxygen titration and weaning with
FreeO2 in patients with acute exacerbation of COPD: a pilot
randomized trial. Int J Chron
Obstruct Pulmon Dis. 2016;11:1983-90.
https://doi.org/10.2147/COPD.S112820
6.
L’Her E, Dias P, Gouillou M, et al. Automatic versus manual oxygen administration in the emergency deÂpartment. Eur Respir J. 2017;50:1602552. https://doi.org/10.1183/13993003.02552-2016
7. Cousins JL, Wark PA, McDonald VM. Acute oxygen therÂapy: a review of
prescribing and delivery practices. Int J Chron Obstruct Pulmon Dis. 2016;11:1067-75. https://doi.org/10.2147/COPD.S103607
8. O’Driscoll
BR. British Thoracic Society. Emergency oxygen audit 2013. Available from:
https://www.brit-thoracic.org.uk/document-library/audit-and-quality-improvement/audit-reports/bts-emergency-oxygen-audit-report-2013/.
Accessed August 15, 2018.
10. Roberts CM, LĂłpez-Campos JL, Pozo-RodrĂguez
F, Hartl S; European COPD Audit team. European hospital adherence to GOLD recommendations for chronic
obstructive pulmonary disease (COPD) exacerbation admissions. Thorax. 2013;68:116971.
https://doi.org/10.1136/thoraxjnl-2013-203465
11. Abdo
WF, Heunks LM. Oxygen-induced hypercapnia
in COPD: myths and facts. Crit Care.
2012;16:323. https://doi.org/10.1186/cc11475